Concussions can be a complex and debilitating condition, impacting millions of individuals each year. Traditional rehabilitation methods often fall short in helping patients regain their pre-injury quality of life. In recent years, the spotlight has turned to neuromodulation techniques as innovative tools that could revolutionize concussion treatment.
These approaches target the brain’s neural pathways, potentially offering relief from persistent symptoms like headaches, dizziness, and cognitive difficulties. By manipulating brain activity through various non-invasive means, neuromodulation might pave the way for more effective recovery protocols. As researchers continue to explore these promising therapies, understanding how they work is critical for anyone affected by concussion-related issues.
Join us as we delve into the exciting world of neuromodulation techniques in concussion rehabilitation. We’ll examine different modalities currently being explored and their potential impact on healing from this widespread injury.
Understanding Neuromodulation and Its Potential in Concussion Treatment
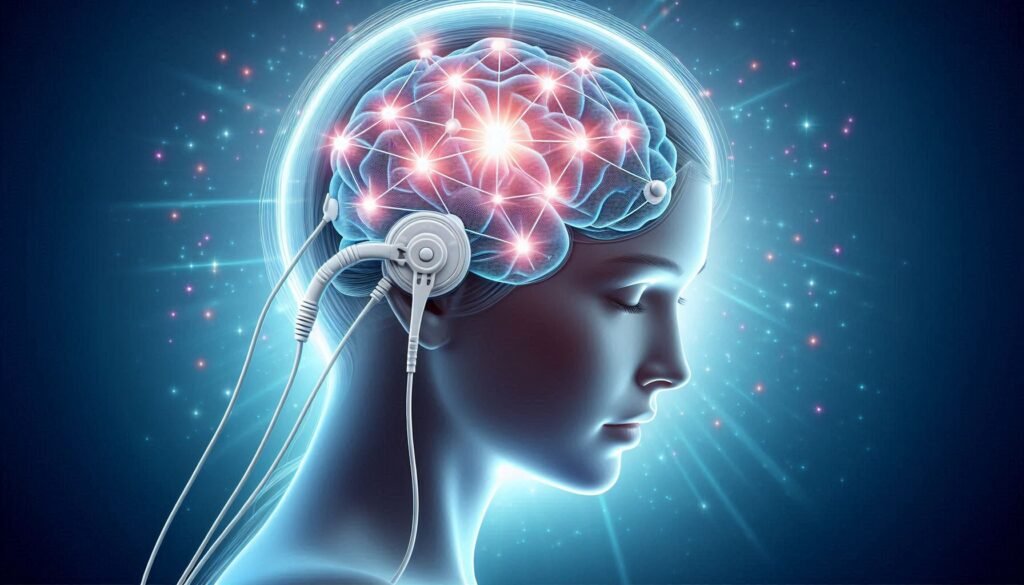
Neuromodulation refers to the process of altering nerve activity through targeted interventions. This innovative approach offers new hope for concussion treatment, focusing on optimizing brain function after injury. By adjusting neural circuits, these techniques may alleviate symptoms and promote recovery.
The human brain is remarkably adaptive, a quality known as neuroplasticity. This ability allows the brain to reorganize itself in response to experiences or injuries. Neuromodulation leverages this trait by stimulating specific areas of the brain, potentially enhancing cognitive and emotional processes compromised by concussions.
Various neuromodulation methods have emerged as candidates for managing post-concussion symptoms. These include non-invasive options like transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS). Each technique aims to restore balance in neural networks disrupted during trauma.
Research continues to explore how these modalities can be integrated into comprehensive rehabilitation programs. As understanding deepens, neuromodulation could become a cornerstone in improving outcomes for individuals suffering from concussive injuries.
Transcranial Magnetic Stimulation (TMS) for Post-Concussion Symptoms
Transcranial Magnetic Stimulation (TMS) is a non-invasive neuromodulation technique gaining traction in concussion rehabilitation. It involves using magnetic fields to stimulate nerve cells in the brain, aiming to enhance neuronal activity and improve cognitive functions. This method shows promise for individuals dealing with persistent post-concussion symptoms.
Research indicates that TMS can alleviate issues like depression, anxiety, and chronic headaches often experienced after concussions. By targeting specific regions of the brain, TMS helps restore normal function and reduces symptom severity. Its applications extend beyond immediate recovery, offering hope for long-term management of post-concussive disorders.
The sessions are typically brief and well-tolerated by patients. Most individuals report no significant discomfort during treatment, making it an appealing option compared to more invasive methods. As research progresses, understanding how TMS interacts with individual neurological profiles will be essential for optimizing its effectiveness.
Ongoing studies continue to explore the ideal frequency and intensity of stimulation required for maximum benefit. With its innovative approach, TMS could redefine standards in concussion care.
Transcranial Direct Current Stimulation (tDCS) in Concussion Recovery
Transcranial Direct Current Stimulation (tDCS) is gaining attention as a promising neuromodulation technique in concussion recovery. This non-invasive method applies a low electrical current to the scalp, which can influence neuronal activity. By modulating brain function, tDCS aims to alleviate post-concussion symptoms such as fatigue, cognitive impairment, and mood disturbances.
Research indicates that tDCS may enhance neuroplasticity—the brain’s ability to adapt and reorganize itself. For individuals recovering from concussions, this could mean improved cognitive functions and better emotional regulation. Studies have shown that targeted stimulation of specific brain regions can lead to significant improvements in symptom management.
One of the key advantages of tDCS is its safety profile and ease of use. Sessions are typically short, lasting around 20-30 minutes, making it suitable for integration into rehabilitation programs. As more clinics adopt this approach, patients increasingly benefit from personalized treatment plans tailored to their unique needs.
While exciting results are emerging from preliminary studies, ongoing research will further clarify the optimal protocols for using tDCS effectively in concussion care.
Vagus Nerve Stimulation: A Novel Approach to Concussion Rehabilitation
Vagus nerve stimulation (VNS) is emerging as a novel approach in concussion rehabilitation. This technique involves delivering electrical impulses to the vagus nerve, which plays a crucial role in regulating various bodily functions, including heart rate and inflammation response. By modulating these processes, VNS has shown promise in alleviating post-concussion symptoms.
Research indicates that VNS may help reduce headaches, anxiety, and mood disturbances commonly associated with concussions. The treatment can be administered through an implanted device or non-invasive methods, making it accessible for different patient needs.
One of the appealing aspects of VNS is its potential neuroprotective effects. It may enhance brain recovery by promoting neuroplasticity—the brain’s ability to adapt and reorganize itself after injury.
As studies continue to explore its efficacy in concussion care, clinicians are optimistic about integrating VNS into comprehensive rehabilitation programs tailored to individual patients’ needs.
Deep Brain Stimulation: Exploring Applications in Severe Cases
Deep brain stimulation (DBS) is an advanced neuromodulation technique gaining traction in managing severe concussion cases. It involves implanting electrodes into specific brain regions to modulate neural activity. This method is typically reserved for patients with persistent and debilitating symptoms that do not respond to conventional therapies.
The targeted areas often include the thalamus or the subthalamic nucleus, which are crucial for motor control and cognitive functions. By delivering electrical impulses, DBS can help normalize abnormal brain rhythms associated with concussion-related issues such as chronic pain, mood disorders, and cognitive impairment.
Research shows promising outcomes for patients experiencing long-term effects from concussions. Many report significant improvements in their quality of life following DBS treatment. Nevertheless, this approach requires careful patient selection due to its invasive nature.
While still considered experimental for concussion rehabilitation, ongoing studies aim to refine techniques and expand applications. As researchers understand more about individual responses to DBS, it holds potential as a transformative option in severe cases of concussion.
Combining Neuromodulation with Cognitive Rehabilitation Techniques
Combining neuromodulation techniques with cognitive rehabilitation presents a promising avenue for enhancing recovery in concussion patients. Neuromodulation can stimulate specific brain regions, potentially improving neural function and connectivity. This stimulation may create an optimal environment for cognitive therapies to take effect.
Cognitive rehabilitation focuses on restoring cognitive abilities affected by concussions, such as memory, attention, and problem-solving skills. When integrated with neuromodulation methods like transcranial magnetic stimulation (TMS), these therapies might yield better outcomes than either approach alone. The synergy between the two could accelerate recovery timelines.
Moreover, personalized treatment plans that include both modalities can be tailored to individual needs. Therapists can assess which areas of cognition are most impacted and adjust the neuromodulatory technique accordingly. This dynamic interaction offers a holistic approach to patient care.
Research is still ongoing in this area, but early findings suggest that combining these approaches may lead to significant improvements in symptom management and overall quality of life for those affected by concussion-related issues.
Safety Considerations and Potential Side Effects of Neuromodulation
Safety is paramount when considering neuromodulation techniques in concussion rehabilitation. These therapies can influence brain activity, which raises questions about their long-term effects. While many studies show promising results, it’s essential to approach these treatments with caution.
Potential side effects vary by method. For example, Transcranial Magnetic Stimulation (TMS) may cause mild headaches or discomfort at the stimulation site. In contrast, transcranial direct current stimulation (tDCS) might lead to skin irritation or a tingling sensation during application.
Patients should also consider individual health factors before starting any neuromodulation therapy. Pre-existing conditions such as epilepsy could heighten risks associated with certain procedures. Therefore, thorough medical evaluations are crucial for safe implementation.
Monitoring patients throughout treatment ensures that any adverse reactions can be promptly addressed. This vigilance helps create a safer environment and enhances the overall effectiveness of the rehabilitation process.
Selecting Appropriate Candidates for Neuromodulation Therapies
Selecting appropriate candidates for neuromodulation therapies is crucial in concussion rehabilitation. Not everyone will benefit from these advanced techniques, making careful evaluation essential. Medical professionals often start with a comprehensive assessment of the individual’s medical history and current symptoms.
Factors such as the severity of the concussion, duration of symptoms, and previous treatment responses play significant roles in determining eligibility. Additionally, psychological factors like anxiety or depression may impact outcomes; addressing these conditions can enhance therapy effectiveness.
It’s also important to consider patient demographics, including age and overall health status. Younger individuals might respond differently than older adults due to variations in brain plasticity.
Collaborative discussions among neurologists, physiotherapists, and psychologists provide a holistic view of each case. This multidisciplinary approach ensures that only those who are most likely to benefit from neuromodulation techniques receive them while minimizing potential risks.
Measuring Outcomes and Efficacy of Neuromodulation in Concussion Care
Measuring the outcomes and efficacy of neuromodulation techniques in concussion care is crucial for understanding their impact. Various assessment tools are used to gauge improvement, including standardized questionnaires, neurocognitive tests, and symptom inventories. These evaluations help clinicians track changes over time.
Technology plays a significant role in this process. Functional MRI (fMRI) and electroencephalography (EEG) can provide real-time insights into brain activity before and after treatment. This data enhances our knowledge of how specific neuromodulation approaches affect neural pathways associated with concussive symptoms.
Patient-reported outcomes also contribute valuable information. Collecting subjective feedback on quality of life, daily functioning, and overall well-being offers a comprehensive view of treatment success from the patient’s perspective.
Clinical trials are essential for establishing evidence-based practices in neuromodulation therapies for concussions. By analyzing large datasets across diverse populations, researchers can determine which techniques yield the best results under varying conditions.
Future Directions in Neuromodulation Research for Concussion Treatment
The landscape of concussion rehabilitation is evolving rapidly, particularly with the integration of neuromodulation techniques. Ongoing research aims to refine these methods for broader application and improved efficacy in treating concussions. Scientists are exploring various parameters such as stimulation frequency, duration, and targeted brain regions to enhance outcomes.
Future studies may also focus on personalized approaches. Tailoring interventions based on individual patient profiles could significantly improve recovery rates. Additionally, there’s a growing interest in combining neuromodulation with other treatments like physical therapy or medication for a more holistic approach.
As technology advances, new devices may emerge that simplify the administration of neuromodulation therapies at home or clinical settings. The objective remains clear: enabling better recovery pathways for those affected by concussions.
With continued exploration into safety protocols and long-term effects, researchers hope to establish robust guidelines that will maximize the benefits while minimizing risks associated with these innovative treatments. As we look ahead, it’s evident that neuromodulation holds promise not just for concussion management but potentially transforming how we address neurological disorders overall.