Concussions have become a prevalent topic in sports, healthcare, and even everyday safety discussions. Yet, the intricate biological processes that unfold after such an injury often remain shrouded in mystery. At the heart of these processes is what researchers call the “neurometabolic cascade following concussion.” This complex series of cellular disruptions can dictate not only immediate symptoms but also long-term recovery outcomes.
Understanding this cascade is crucial for athletes, coaches, medical professionals, and anyone interested in brain health. It reveals how a seemingly singular event—a blow to the head—can trigger a chain reaction affecting energy production, neurotransmitter balance, and inflammation levels within the brain. By delving into each stage of this cascade, we gain valuable insights into why some individuals recover swiftly while others face prolonged challenges.
Join us as we explore the fascinating world of neurometabolism post-concussion and uncover essential information for better prevention strategies and rehabilitation methods.
The Immediate Cellular Response to Concussive Impact
When a concussion occurs, the brain experiences a sudden and forceful impact. This disruption triggers an immediate cellular response that sets off a chain reaction within neural tissue. Neurons react swiftly to the trauma, leading to mechanical stress and potential damage.
In this acute phase, calcium ions flood into the cells while potassium ions leak out. This ionic imbalance creates instability in neuronal membranes and disrupts normal electrical signaling. As neurons struggle to maintain homeostasis, they initiate various metabolic processes aimed at restoring balance.
Simultaneously, neurotransmitter release surges as the brain attempts to communicate changes rapidly across synapses. Glutamate levels spike significantly during this time, which can further exacerbate excitotoxicity—the process where excessive stimulation leads to neuronal injury or death.
This initial cellular response is critical but also highly vulnerable. The brain’s delicate ecosystem becomes destabilized, setting the stage for subsequent phases of the neurometabolic cascade following concussion.
Phases of the Neurometabolic Cascade: From Minutes to Weeks
The neurometabolic cascade following concussion unfolds in distinct phases, each with varying timeframes and cellular effects. Initially, within minutes of the injury, there is a rapid release of neurotransmitters. This spike can lead to excitotoxicity, where excessive stimulation damages neurons.
As hours pass, metabolic changes take center stage. The brain’s energy demands increase dramatically while its ability to produce ATP—the energy currency—becomes compromised. This creates an energy deficit that affects cellular function.
Over the ensuing days, inflammatory responses begin to manifest. Activated glial cells release pro-inflammatory cytokines that further disrupt neuronal communication and contribute to swelling in affected areas.
By weeks later, these processes may evolve into chronic conditions if not properly managed. Long-term disruptions in metabolism can hinder recovery and increase vulnerability to subsequent injuries or complications down the line. Understanding this timeline is crucial for effective diagnosis and treatment strategies post-concussion.
Energy Crisis and Mitochondrial Dysfunction in Concussed Brains
The neurometabolic cascade following concussion triggers a complex series of cellular events, one of the most critical being an energy crisis in the brain. When a concussive impact occurs, neurons rapidly deplete their energy stores. This depletion results from an increased demand for ATP production to facilitate repair processes and restore homeostasis.
Mitochondria, known as the powerhouse of cells, become dysfunctional during this phase. They struggle to meet the elevated energy demands caused by excitatory neurotransmitter release and neuronal swelling. Consequently, mitochondrial respiration is impaired, leading to further ATP shortages.
As mitochondria falter, reactive oxygen species (ROS) levels rise dramatically. These harmful molecules can damage cellular components like lipids and proteins, exacerbating injury severity and prolonging recovery times.
This dual issue—energy supply failure coupled with oxidative stress—creates a vicious cycle that affects not just immediate healing but also long-term cognitive functioning after concussion. Addressing mitochondrial health could play a vital role in improving outcomes for those affected by traumatic brain injuries.
Ionic Imbalances and Their Role in Post-Concussion Symptoms
Ionic imbalances play a critical role in the aftermath of a concussion. When the brain sustains an injury, there is a disruption in the balance of ions such as sodium, potassium, calcium, and chloride. These ions are vital for maintaining normal cellular function and communication.
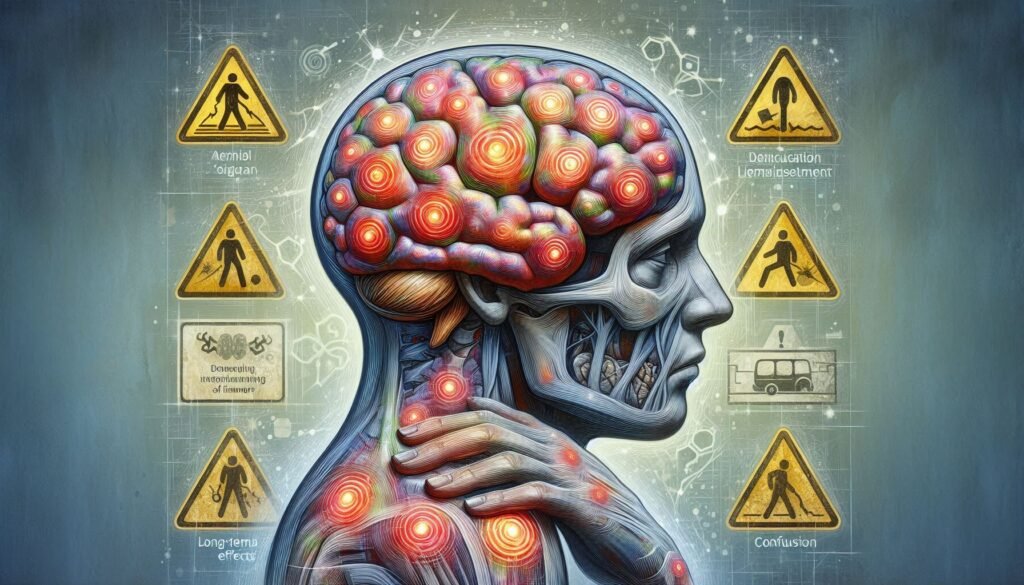
After impact, neurons experience excessive excitability due to an influx of calcium ions. This can lead to overstimulation and increased metabolic demands on cells. The result is often debilitating post-concussion symptoms like headaches, dizziness, and cognitive difficulties.
Additionally, disruptions in potassium ion levels can impair neuronal repolarization after firing. This creates further complications in signaling pathways essential for recovery processes. Consequently, individuals may experience prolonged cognitive deficits or mood disturbances.
Restoring ionic balance becomes crucial during rehabilitation efforts following a concussion. Understanding these imbalances helps guide both diagnostic assessments and therapeutic interventions aimed at alleviating symptoms effectively.
Neurotransmitter Disruptions During the Acute Phase of Injury
Following a concussion, neurotransmitter systems experience significant disruptions. These chemical messengers are crucial for communication between neurons. When a concussive impact occurs, the delicate balance of neurotransmitters is thrown into disarray.
Glutamate levels often rise sharply during this acute phase. This excitatory neurotransmitter can become toxic in excess amounts, leading to overstimulation of receptors and potential neuronal damage. The brain’s ability to maintain homeostasis is compromised, making recovery more complex.
Simultaneously, gamma-aminobutyric acid (GABA), the primary inhibitory neurotransmitter, may not function effectively due to altered receptor sensitivity or decreased production. This imbalance contributes further to cognitive dysfunction and mood disturbances commonly seen after injury.
The resultant cascade affects various brain regions involved in memory and emotion regulation. Understanding these disruptions offers insights into post-concussion symptoms and guides therapeutic approaches aimed at restoring normal neurotransmitter function during recovery.
Neuroinflammatory Responses and Their Long-Term Implications
Neuroinflammation is a critical response to concussion that can significantly impact recovery. Following an injury, the brain’s immune system activates microglia and astrocytes. These cells work to repair damage but can also release pro-inflammatory cytokines.
This inflammatory cascade may lead to persistent symptoms like headaches, dizziness, and cognitive difficulties. The duration and intensity of neuroinflammation vary among individuals, influenced by factors such as genetics and prior injuries.
Chronic neuroinflammatory responses have been linked to long-term conditions like chronic traumatic encephalopathy (CTE) or other neurodegenerative diseases. Research suggests that prolonged inflammation could result in neuronal cell death and synapse loss over time.
Understanding these mechanisms is vital for developing effective interventions aimed at reducing inflammation after concussion. Targeting this aspect of the neurometabolic cascade following concussion could pave the way for improved outcomes in affected individuals.
The Vulnerability Window: Risks of Repeat Injury During Recovery
After a concussion, the brain enters a state of heightened vulnerability. This period, often referred to as the “vulnerability window,” can last days to weeks and is critical for recovery. During this time, the risk of sustaining another injury increases significantly.
When an individual experiences a second concussion before fully recovering from the first, it can lead to severe complications. This phenomenon is known as second impact syndrome (SIS). Symptoms may escalate rapidly and could result in long-lasting damage or even fatal outcomes.
The neurometabolic cascade following concussion plays a crucial role here. The initial metabolic disruptions impair cellular function, making neurons more sensitive to additional trauma. The brain’s protective mechanisms are compromised during this phase.
Athletes and individuals involved in contact sports must be particularly cautious. Adhering strictly to protocols for return-to-play ensures that they do not jeopardize their health by returning too soon after an injury.
Biomarkers of Neurometabolic Disruption: Diagnostic Potential
Biomarkers play a crucial role in understanding the neurometabolic cascade following concussion. They serve as measurable indicators of cellular disruption and can provide insights into the severity of injury. Researchers have identified specific proteins, metabolites, and inflammatory markers that may reflect changes occurring in the brain after concussive events.
One promising area is the study of glial fibrillary acidic protein (GFAP) and S100B levels. Both are linked to astrocytic activation and neuronal damage. Elevated concentrations after a concussion can signal ongoing neuroinflammation or cell death, helping clinicians assess recovery trajectories more accurately.
Additionally, metabolic by-products such as lactate may indicate energy deficits within brain cells post-injury. Monitoring these biomarkers could enhance diagnostic precision, allowing for tailored treatment plans based on individual patient needs.
The potential for using biomarkers extends beyond immediate diagnosis; they might also aid in predicting long-term outcomes related to cognitive function and overall health after concussion. This opens avenues for early interventions aimed at minimizing lasting effects on neurological wellbeing.
Therapeutic Interventions Targeting the Neurometabolic Cascade
Therapeutic interventions targeting the neurometabolic cascade following concussion aim to address the cellular disturbances that occur after injury. One promising strategy is the use of neuroprotective agents, such as antioxidants and anti-inflammatory medications. These compounds can help mitigate oxidative stress and reduce inflammation in injured brain tissue.
Another approach involves metabolic support therapies. Nutritional interventions that provide essential nutrients like omega-3 fatty acids, vitamins C and E, and magnesium have shown potential in promoting recovery. These nutrients play crucial roles in mitochondrial function and energy metabolism, which are often compromised after a concussion.
Cognitive rest combined with gradual return-to-activity protocols helps manage symptoms while allowing for healing. Therapies focused on vestibular rehabilitation or cognitive behavioral therapy may also be beneficial for individuals experiencing persistent post-concussive symptoms.
Emerging research into biofeedback techniques suggests they could enhance self-regulation of brain function during recovery. These innovative treatments focus on training individuals to modulate their physiological responses to stressors effectively.
Long-Term Cellular Recovery and Potential for Neuroprotection
Long-term cellular recovery following a concussion is a complex process influenced by various factors. The neurometabolic cascade initiates immediate disruptions, but as time progresses, the brain begins to repair itself. Understanding this recovery phase is essential for both patients and healthcare providers.
Neuroprotection strategies are increasingly being researched to support this recovery. Enhancing mitochondrial function plays a crucial role in restoring energy balance within cells. Nutritional interventions and specific medications may help mitigate energy deficits caused by the initial injury.
Furthermore, promoting neuroplasticity—the brain’s ability to reorganize itself—can facilitate better outcomes post-injury. This includes therapies that encourage cognitive engagement and physical rehabilitation tailored for concussed individuals.
Monitoring biomarkers associated with the neurometabolic cascade can also guide treatment plans, ensuring timely intervention when necessary. Educating athletes about the risks of returning too soon can help prevent additional injuries during vulnerable periods of recovery.
As we deepen our understanding of the neurometabolic cascade following concussion, it opens doors for innovative treatments aimed at enhancing long-term cellular health and reducing potential complications from repeated trauma. The future looks promising as research continues to unfold in this critical area of neurological health.