Whiplash and concussion are two injuries that often overlap, especially in high-impact scenarios like car accidents or sports. Both conditions can lead to a complex web of symptoms, making it challenging for patients and healthcare providers alike to navigate the healing process. While whiplash typically affects the neck due to sudden movement, concussions impact brain function. However, what happens when these two injuries occur simultaneously? Understanding the nuances of concussion symptoms in whiplash-associated disorders is crucial for effective diagnosis and treatment.
With so many shared symptoms—such as headaches, dizziness, and cognitive difficulties—recognizing which condition is at play can be daunting. This blog will delve into the intricate relationship between whiplash and concussion while exploring common symptoms, diagnostic challenges, neurological mechanisms behind their overlaps, and more. Whether you’re seeking information for yourself or a loved one dealing with these issues, this guide aims to clarify your path toward recovery.
Understanding the Relationship Between Whiplash and Concussion
Whiplash and concussion often occur together, especially in situations involving rapid head and neck movements. Whiplash is primarily an injury to the cervical spine, typically caused by sudden acceleration-deceleration forces. This trauma can lead to various symptoms related to both the neck and neurological function.
Concussions, on the other hand, result from a blow or jolt to the head that disrupts normal brain activity. The mechanical forces involved in whiplash can also affect the brain’s positioning within the skull, increasing susceptibility to concussive symptoms.
Patients experiencing these two conditions may report overlapping signs like headaches and dizziness. However, understanding each condition’s unique aspects is crucial for effective treatment strategies.
The bidirectional nature of these injuries means that addressing one without considering the other could impede recovery efforts. A comprehensive approach is essential for managing both whiplash-related pain and concussion symptoms effectively.
Common Symptoms Shared by Whiplash and Concussion Injuries
Whiplash and concussion injuries often present overlapping symptoms, which can complicate diagnosis and treatment. Both conditions may lead to headaches, a common complaint among individuals experiencing whiplash or concussions. The nature of these headaches can vary but is frequently described as tension-like or migraine-like.
Another shared symptom is cognitive dysfunction. Patients may report difficulties with memory, concentration, and processing information following either injury. This impairment can significantly impact daily activities and quality of life.
Dizziness also appears in both cases. Whether stemming from neck strain related to whiplash or neurological disturbances associated with a concussion, dizziness can be disorienting for those affected.
Fatigue is another overlap worth noting. Individuals suffering from either condition often experience increased tiredness due to the physical toll of their injuries as well as sleep disturbances that accompany them. Understanding these shared symptoms plays a crucial role in the management of both whiplash-associated disorders and concussions.
Neurological Mechanisms Underlying Symptom Overlap
The overlap of concussion symptoms in whiplash-associated disorders is rooted in complex neurological mechanisms. Both conditions can disrupt normal brain function, leading to a range of cognitive and physical manifestations.
In concussions, the primary issue often lies within the brain’s neural pathways due to trauma-induced changes. These alterations affect neurotransmitter release, resulting in headaches, dizziness, and memory issues. Similarly, whiplash injuries can cause strain on neck muscles and ligaments that influence cranial blood flow and nerve signaling.
Moreover, both conditions may trigger an inflammatory response that exacerbates symptoms. Neuroinflammation from either injury type can lead to increased sensitivity to pain and further cognitive impairments.
Shared vestibular pathways play a critical role as well. Disruptions in these areas can simultaneously produce balance problems or visual disturbances regardless of whether the origin is a concussion or whiplash injury.
Diagnostic Challenges in Differentiating Whiplash from Concussion
Diagnosing whiplash and concussion can be particularly challenging due to overlapping symptomatology. Both conditions frequently arise from similar mechanisms, such as motor vehicle accidents or sports injuries. This similarity often leads to confusion in clinical assessment.
Symptoms like headaches, dizziness, and cognitive difficulties are common in both disorders. Without clear diagnostic tools, healthcare providers may struggle to pinpoint which condition a patient is experiencing. Relying solely on patient-reported symptoms can complicate matters further.
Additionally, the timing of symptom onset adds another layer of complexity. Whiplash symptoms might present immediately following an injury, while concussion-related symptoms could take hours or even days to manifest fully. This delayed reaction makes it hard for clinicians to establish a definitive diagnosis based on initial observations alone.
Imaging techniques like MRIs and CT scans do not always reveal abnormalities linked specifically to either condition, limiting their effectiveness as diagnostic aids. As a result, comprehensive assessments that consider the full spectrum of signs are crucial for accurate differentiation between these two injuries.
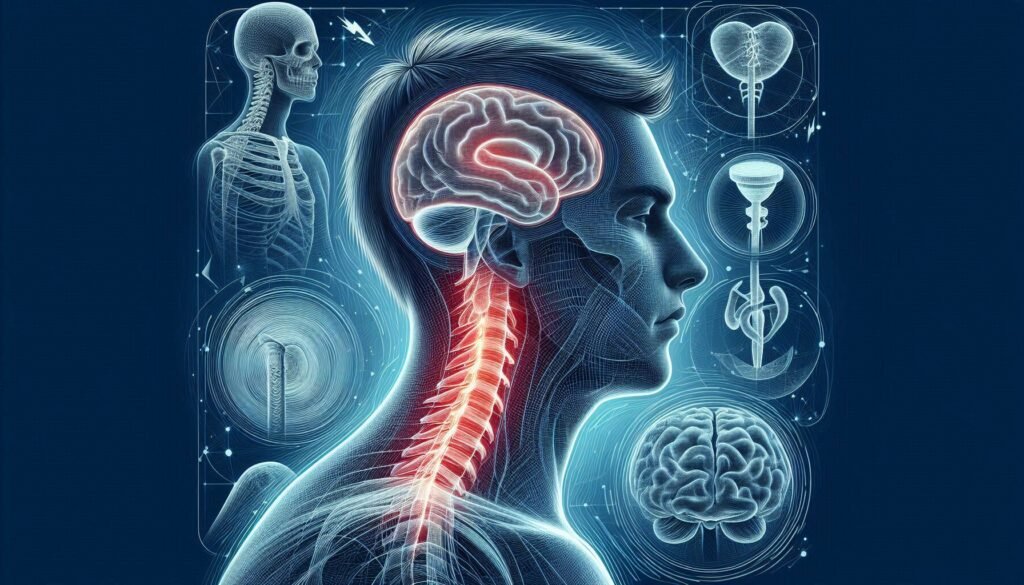
The Role of Cervical Spine Dysfunction in Concussion-Like Symptoms
Cervical spine dysfunction can significantly contribute to concussion-like symptoms in individuals with whiplash-associated disorders. The cervical spine consists of vertebrae that support the head and protect the spinal cord. When these structures are injured, it may lead to pain, limited mobility, and nerve irritation.
Altered biomechanics in the neck can impact how the brain receives signals from the body. This disruption may mimic or exacerbate symptoms commonly associated with concussions, such as headaches, dizziness, and cognitive difficulties. As a result, patients often find themselves struggling to differentiate between true concussion effects and those arising from cervical issues.
Muscle tension surrounding the cervical region can also play a role. Tight muscles can irritate nerves leading to sensations similar to those experienced during a concussion. Moreover, this discomfort may limit physical activity further complicating recovery.
Addressing cervical spine dysfunction is crucial for effective treatment planning. By targeting these underlying issues through appropriate therapy techniques like manual manipulation or rehabilitation exercises, healthcare providers can help alleviate overlapping symptoms effectively.
Vestibular and Oculomotor Disturbances in Whiplash and Concussion
Vestibular and oculomotor disturbances often emerge in individuals with whiplash-associated disorders or concussions. These symptoms can significantly impact daily functioning, making it vital to recognize their presence early on.
The vestibular system is responsible for balance and spatial orientation. When disrupted, patients may experience dizziness, vertigo, or unsteadiness. Such sensations can be distressing and lead to difficulties in maintaining equilibrium during routine activities.
Oculomotor dysfunction involves issues with eye movement control. Patients might struggle with tracking objects smoothly or focusing effectively. Symptoms like double vision or difficulty shifting gaze from near to far can exacerbate the challenges faced by those already coping with pain and discomfort.
Both disturbances share common neurological pathways but stem from different origins related to injury mechanisms. Understanding these nuances is essential for tailored rehabilitation strategies that address each patient’s unique symptom profile.
Treatment Approaches for Managing Overlapping Symptoms
Managing overlapping symptoms of concussion and whiplash requires a tailored approach. Physical therapy is often one of the first lines of treatment. Therapists work to improve mobility, strength, and coordination, focusing on the cervical spine’s health.
Cognitive behavioral therapy (CBT) can also be beneficial. CBT helps patients address emotional responses to their injuries while providing coping strategies for anxiety or depression that may accompany their physical symptoms.
Medication management may play a role too. Pain relievers or anti-inflammatory drugs can help alleviate discomfort from both conditions, while antidepressants might be prescribed for mood stabilization.
Integrating vestibular rehabilitation can effectively address dizziness and balance issues common in both disorders. This specialized form of therapy focuses on improving balance through specific exercises designed to enhance sensory integration and motor control.
The Importance of Multidisciplinary Care in Complex Cases
Multidisciplinary care is essential for individuals experiencing concussion symptoms in whiplash-associated disorders. A collaborative approach ensures that all aspects of a patient’s condition are addressed, leading to more comprehensive treatment plans.
Different specialists bring unique expertise to the table. For instance, neurologists can assess cognitive function while physical therapists focus on restoring mobility and strength. This teamwork creates a holistic understanding of each patient’s needs.
Coordination among healthcare providers enhances communication about symptom management and recovery strategies. Regular meetings allow professionals to share insights, ensuring that treatment remains aligned with the patient’s evolving condition.
Moreover, patients benefit from personalized care tailored to their specific challenges. As they navigate complex symptoms from both injuries, having access to diverse medical perspectives fosters better outcomes and improves overall quality of life during recovery.
Prognosis and Recovery Trajectories in Combined Injuries
The prognosis for individuals suffering from both concussion symptoms in whiplash-associated disorders varies significantly. Factors such as the severity of injuries, individual health status, and timely intervention play crucial roles in recovery trajectories. Some patients may experience a relatively swift return to normal function, while others face prolonged symptoms.
Research indicates that those with combined injuries often report persistent cognitive issues, headaches, and neck pain. The complex interplay between these symptoms can complicate treatment processes and delay recovery times. Early diagnosis is critical for optimal outcomes.
A multidisciplinary approach tends to yield better results. Treatment might involve physical therapy, cognitive rehabilitation, and psychological support tailored specifically to address overlapping symptoms effectively. Collaboration among healthcare providers ensures that all aspects of injuries are managed comprehensively.
Recovery timelines also differ based on adherence to treatment protocols and lifestyle modifications. Patients who actively participate in their care tend to show improved prognoses over time compared to those who do not engage fully with their recovery process.
Prevention Strategies for Whiplash and Concussion in High-Risk Activities
Preventing whiplash and concussion in high-risk activities is essential for reducing the incidence of these injuries. Awareness plays a crucial role. Individuals engaging in sports or activities with a higher likelihood of head or neck trauma should be educated on proper techniques and safety protocols.
Wearing appropriate protective gear, such as helmets and neck braces, can significantly mitigate risks associated with concussive impacts. For athletes, following rules designed to enhance player safety is critical. Coaches and trainers should emphasize the importance of not playing through symptoms, encouraging immediate evaluation if an injury occurs.
Conducting regular training sessions that focus on strengthening neck muscles can also help reduce vulnerability to whiplash injuries. Additionally, promoting safe driving practices can lower the risk of motor vehicle accidents—common causes of both whiplash and concussions.
Creating an environment that prioritizes health education raises awareness about the signs and symptoms associated with these conditions. Early intervention can lead to timely treatment and better long-term outcomes for those affected by concussion symptoms in whiplash-associated disorders. This proactive approach helps safeguard individuals against potential complications stemming from these intertwined injuries.