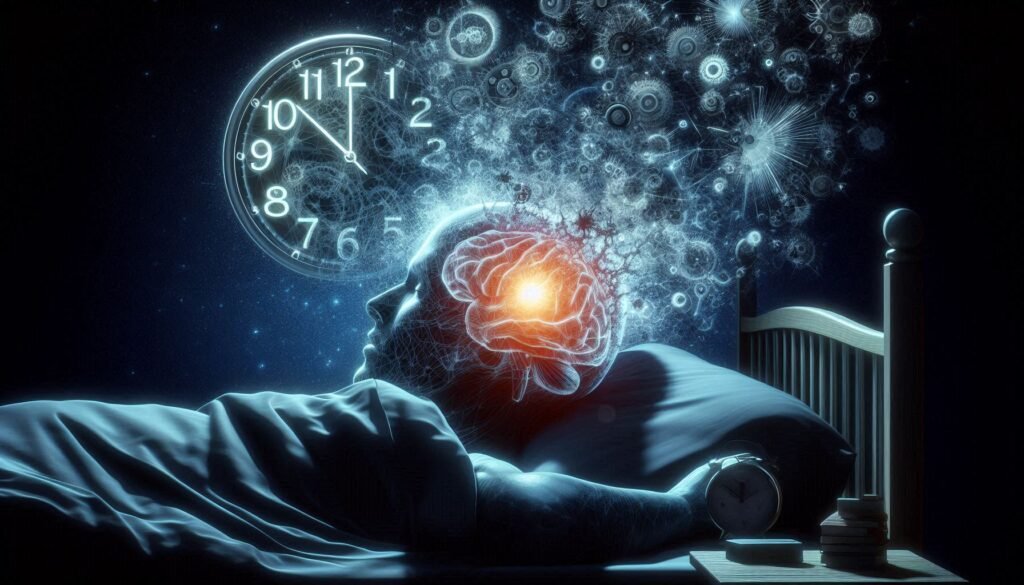
Concussions are often associated with physical symptoms like headaches, dizziness, and confusion. However, their impact extends far beyond immediate injuries to the brain. One of the lesser-known consequences is how a concussion can disrupt our natural circadian rhythm—the internal clock that regulates sleep-wake cycles. This disruption can lead to significant sleep disturbances, ultimately affecting cognitive recovery and daily functioning.
Understanding the complex relationship between concussions and circadian rhythm is essential for effective management and recovery. With millions affected each year by traumatic brain injuries, recognizing these subtle yet impactful changes in sleep patterns becomes increasingly important for healthcare providers and patients alike. Join us as we delve into this nuanced topic exploring the interplay between concussion’s impact on circadian rhythm, its biological underpinnings, treatment options available today, and strategies to restore normalcy in our everyday lives.
Understanding Circadian Rhythm and Its Vulnerability to Brain Injury
Circadian rhythm refers to the body’s internal clock that regulates various physiological processes over a 24-hour cycle. It influences sleep patterns, hormone release, and even metabolism. This intricate system is primarily controlled by a group of neurons in the hypothalamus called the suprachiasmatic nucleus (SCN).
When brain injury occurs, such as from a concussion, these neural pathways can be disrupted. This disruption may lead to misalignment between our biological rhythms and external environmental cues like light and darkness. As a result, individuals may experience difficulties falling asleep or staying awake during typical hours.
The vulnerability of circadian rhythm to brain injuries underscores its importance for overall health. Sleep disruptions caused by concussions can contribute to prolonged recovery times and impact cognitive function significantly. Understanding this connection helps in recognizing why proper management of sleep disturbances is crucial following an injury.
Awareness of how concussions affect circadian rhythm not only aids in treatment but also emphasizes the need for preventive measures during high-risk activities.
Common Sleep-Wake Cycle Disruptions Following Concussion
Following a concussion, many individuals experience significant disruptions in their sleep-wake cycles. One of the most common issues is insomnia, where victims struggle to fall asleep or stay asleep throughout the night. This can lead to daytime fatigue and exacerbate cognitive difficulties.
Another frequent disruption is hypersomnia, characterized by excessive daytime sleepiness. Those affected may find it challenging to remain alert during daily activities, impacting their productivity and overall quality of life. The unpredictability of these fluctuations adds another layer of difficulty for those recovering from a brain injury.
Circadian rhythm disturbances also manifest as irregular sleep patterns. People might experience fragmented sleep or shift between periods of wakefulness and restlessness at odd hours. These changes can confuse one’s biological clock, making recovery even more arduous.
Moreover, some individuals report vivid nightmares or altered dreams post-concussion. Such experiences not only interrupt restorative sleep but can also contribute to anxiety about bedtime, creating a vicious cycle that hinders recovery efforts.
Neurobiological Mechanisms of Circadian Rhythm Disturbances
Circadian rhythms are regulated by a complex interplay of neural mechanisms. The suprachiasmatic nucleus (SCN) in the hypothalamus serves as the brain’s master clock, coordinating various physiological processes aligned with day-night cycles. When a concussion occurs, this delicate system can be disrupted.
Neurotransmitters and hormones play critical roles in maintaining circadian balance. For instance, serotonin influences mood and sleep patterns while melatonin regulates sleep onset. After a brain injury, alterations in these neurotransmitter levels can lead to significant disturbances.
Inflammation resulting from a concussion may also affect circadian regulation. Neuroinflammation is known to disrupt signaling pathways that govern the body’s internal clock, potentially leading to irregular sleep-wake cycles.
Moreover, structural damage within specific brain regions can impair their function in regulating circadian rhythms. This disruption not only affects restorative sleep but also has cascading effects on cognitive abilities and emotional well-being for individuals recovering from concussions.
The Role of Melatonin Production in Post-Concussion Sleep Issues
Melatonin is a hormone that regulates sleep-wake cycles, playing a crucial role in maintaining our circadian rhythm. Following a concussion, melatonin production can be disrupted, leading to sleep issues. This disruption may stem from changes in the brain’s neural pathways and hormonal balance after an injury.
Research indicates that individuals with concussions often experience lower levels of melatonin at night. This deficiency can lead to difficulties falling asleep or staying asleep, exacerbating fatigue and cognitive impairment associated with post-concussion syndrome.
In addition to nocturnal secretion disruptions, exposure to blue light from screens before bed further hampers melatonin release. As many people use electronic devices for entertainment or work late into the evening, this creates a vicious cycle affecting sleep quality.
Addressing these melatonin issues is essential for recovery. Restoring normal melatonin levels can support better sleep patterns and enhance overall healing after a concussion. Understanding this relationship helps inform effective management strategies moving forward.
Impact of Circadian Disruption on Cognitive Recovery and Daily Functioning
Circadian disruption significantly affects cognitive recovery after a concussion. When the body’s internal clock is thrown off, it can hinder essential processes like memory consolidation and attention span. This impairment often leads to difficulties in focusing on tasks or retaining new information.
Individuals may also experience increased fatigue during the day due to disrupted sleep patterns. This lack of restorative sleep not only impacts energy levels but can exacerbate mood swings and irritability, further complicating recovery efforts.
Daily functioning becomes a challenge as well, with common activities feeling overwhelming or exhausting. Everyday responsibilities might seem insurmountable when cognitive clarity diminishes.
The ripple effect extends beyond personal well-being into social interactions and professional life. Struggles with communication and decision-making skills can create barriers, hindering one’s ability to engage fully in work or relationships while navigating post-concussion symptoms.
Diagnostic Approaches for Assessing Circadian Rhythm Disorders
Diagnosing circadian rhythm disorders following a concussion involves a combination of subjective and objective methods. Clinicians often begin by taking a detailed medical history, focusing on sleep patterns, daily routines, and symptoms experienced after the injury. Patient interviews can reveal crucial insights into changes in sleep-wake cycles.
Actigraphy is another valuable tool for assessment. This non-invasive method uses wrist-worn devices that track movement and light exposure over extended periods. The collected data helps to identify irregularities in activity levels associated with the individual’s circadian rhythm.
Polysomnography (PSG) may also be employed when more comprehensive analysis is needed. This overnight sleep study measures various physiological signals while the patient sleeps, providing information about sleep architecture and disturbances.
Additionally, questionnaires like the Pittsburgh Sleep Quality Index (PSQI) or Epworth Sleepiness Scale can help gauge overall sleep quality and daytime alertness. These assessments together create a well-rounded picture of how concussion affects an individual’s circadian rhythm.
Non-Pharmacological Interventions for Restoring Sleep-Wake Cycles
Non-pharmacological interventions play a crucial role in restoring sleep-wake cycles for those affected by concussion’s impact on circadian rhythm. Behavioral therapies, such as cognitive-behavioral therapy for insomnia (CBT-I), have shown promising results. This approach helps individuals identify and change negative thought patterns surrounding sleep.
Another effective method is establishing a consistent daily routine. Keeping regular sleep and wake times reinforces the body’s internal clock, which can be disrupted after a concussion. A stable schedule promotes better alignment with natural circadian rhythms.
Mindfulness practices, including meditation and relaxation techniques, can also enhance overall sleep quality. These methods reduce stress and anxiety levels that often accompany post-concussion symptoms, aiding in achieving more restful slumber.
Environmental modifications are essential too; creating an optimal sleeping environment can make a difference. Darkening rooms at night while ensuring exposure to natural light during the day can significantly improve the body’s ability to regulate its internal clock effectively.
Medication Options for Managing Post-Concussion Sleep Disturbances
Medication options for managing post-concussion sleep disturbances can be varied and tailored to individual needs. Commonly prescribed medications include sedatives such as benzodiazepines, which may help induce sleep but come with risks of dependency and tolerance. Careful monitoring by a healthcare provider is essential when using these drugs.
Antidepressants like trazodone are also frequently utilized due to their dual action on mood regulation and sleep enhancement. They tend to have fewer side effects compared to traditional sleeping pills, making them a popular choice among physicians.
Melatonin supplements offer another option. This naturally occurring hormone regulates the sleep-wake cycle and can help restore balance after brain injury. Dosage should be carefully adjusted under medical guidance for optimal results.
Some individuals may benefit from anticonvulsants or atypical antipsychotics in specific cases where other treatments haven’t been effective. These medications require close supervision due to potential side effects but can provide relief when necessary.
Light Therapy and Other Chronotherapeutic Approaches
Light therapy is an emerging treatment for sleep disturbances resulting from a concussion’s impact on circadian rhythm. This approach uses specific wavelengths of light to influence the body’s internal clock, promoting alertness during the day and improving sleep quality at night. By carefully timing exposure to bright light, individuals can help reset their biological clocks.
Chronotherapeutic approaches extend beyond just light therapy. Behavioral strategies play a crucial role as well. Maintaining consistent sleep schedules, minimizing screen time before bed, and creating a calming bedtime routine can enhance overall sleep hygiene.
Additionally, optimizing environmental factors—such as reducing noise and regulating room temperature—can contribute positively to better rest. Mindfulness practices like meditation or yoga may also alleviate stress that interferes with sleep.
For many patients recovering from concussions, integrating these methods into daily life offers a holistic path toward restoring regular circadian rhythms while managing symptoms effectively over time.
Long-Term Management Strategies for Persistent Circadian Issues
Managing the long-term consequences of concussion’s impact on circadian rhythm requires a comprehensive approach. First, establishing a consistent sleep schedule can be beneficial. Going to bed and waking up at the same time every day helps reinforce your body’s natural clock.
Incorporating relaxation techniques such as mindfulness or yoga can also promote better sleep quality. These practices reduce stress levels, making it easier for individuals to unwind before bedtime.
Nutritional habits play an essential role too; avoiding heavy meals close to bedtime and limiting caffeine intake can improve overall sleep hygiene.
Regular physical activity is another crucial factor, but it’s vital to tailor exercise routines based on personal comfort levels post-concussion. Gentle activities like walking or swimming may help without overwhelming the nervous system.
Maintaining good light exposure during the day supports melatonin production in alignment with natural cycles, aiding both mood and energy levels. Collaborating closely with healthcare professionals ensures that any persistent issues are addressed effectively.
By incorporating these strategies into daily life, those affected by concussion-related circadian disturbances can work towards restoring balance and improving their overall well-being.