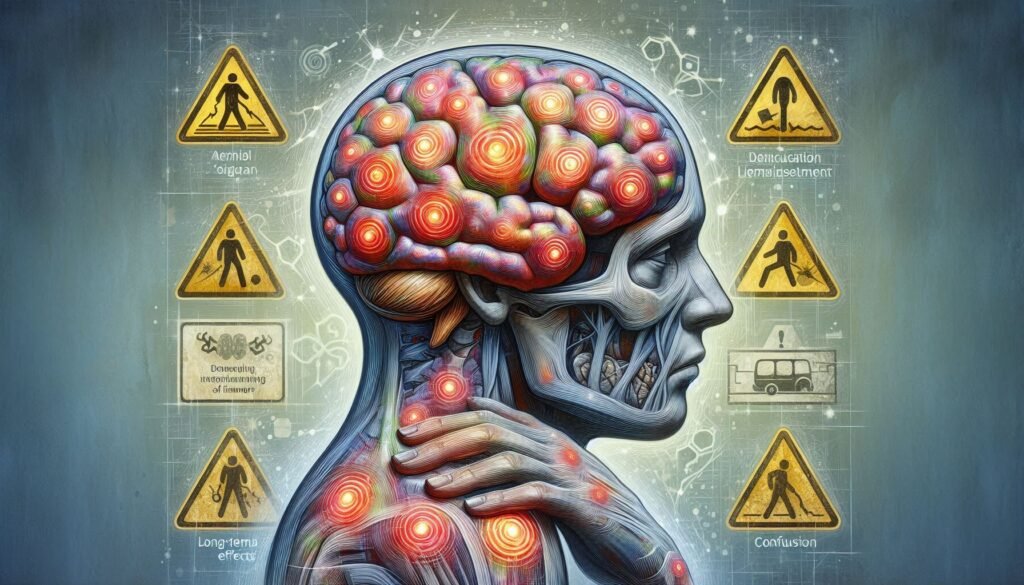
Head injuries, whether from sports, accidents, or falls, can have far-reaching consequences beyond the initial trauma. One of the lesser-known but significant effects is the disruption of neurotransmitter balance in the brain. Neurotransmitters are chemical messengers that play a crucial role in regulating mood, cognition, and overall brain function. When these delicate systems are thrown off balance after a head injury, individuals may experience a range of symptoms that can hinder their recovery.
Understanding how neurotransmitter imbalances occur and their implications on mental health is essential for anyone navigating life post-injury. From mood disturbances to cognitive decline, these imbalances can significantly impact daily functioning and quality of life. This blog delves into common disruptions following concussions and explores strategies for addressing them—offering insights into a path toward healing both physically and mentally. Join us as we unravel this complex topic to better equip ourselves with knowledge about neurotransmitter imbalances after head injury.

Understanding the Role of Neurotransmitters in Brain Function
Neurotransmitters are essential for effective brain function, acting as the brain’s communication network. These chemical messengers transmit signals between neurons, facilitating everything from muscle movement to emotional regulation. Each neurotransmitter has a specific role and effect on our behavior and cognitive processes.
There are various types of neurotransmitters, including excitatory ones like glutamate that stimulate activity in the brain, and inhibitory ones like GABA that calm neural responses. This balance is crucial; too much excitation can lead to overstimulation, while excessive inhibition may result in sluggishness or anxiety.
Dopamine plays an important role in motivation and reward processing. It significantly affects mood and pleasure sensations. On the other hand, serotonin regulates mood stability and feelings of happiness.
Understanding how these neurotransmitters interact helps shed light on their importance in recovery after head injuries. Disrupting this balance can lead to complications affecting mental health and cognitive abilities long after the initial injury has occurred.
Common Neurotransmitter Disruptions Following Concussion
Following a concussion, the delicate balance of neurotransmitters in the brain can be significantly disrupted. This imbalance often leads to various cognitive and emotional challenges. Neurotransmitters like glutamate, dopamine, serotonin, and GABA may all experience alterations that impact recovery.
Glutamate plays a crucial role in excitatory signaling within the brain. After head injury, its levels can surge excessively, leading to excitotoxicity—a condition that damages neurons and exacerbates symptoms.
Dopamine disruption is also common post-concussion. Changes in dopamine levels can result in mood swings and difficulties with concentration or motivation. The emotional toll can be profound for many individuals.
Serotonin disturbances are frequently observed as well. These imbalances have been linked to increased risks of anxiety and depression after an injury. Additionally, GABA changes contribute to heightened anxiety disorders and sleep problems following concussive events. Understanding these disruptions is vital for guiding effective treatment strategies during recovery.
The Impact of Glutamate Excitotoxicity on Brain Health
Glutamate is the brain’s primary excitatory neurotransmitter, playing a vital role in synaptic transmission and plasticity. However, after a head injury, excessive glutamate release can lead to excitotoxicity. This condition occurs when neurons are overstimulated, causing cellular damage or death.
Excitotoxicity triggers an influx of calcium ions into the cells. The overload disrupts normal cell function and initiates harmful biochemical processes. Over time, this cascade can contribute to neuroinflammation and long-term cognitive deficits.
The relationship between glutamate and oxidative stress further complicates recovery from a head injury. Increased free radicals generated during excitotoxic events may exacerbate neuronal damage, creating a vicious cycle of impairment.
Addressing glutamate imbalances becomes crucial for brain health post-injury. Therapeutic strategies targeting glutamatergic pathways offer potential avenues for mitigating these effects and supporting recovery efforts in individuals experiencing neurotransmitter imbalances after head injury.
Dopamine Dysregulation: Effects on Mood and Cognition
Dopamine is a crucial neurotransmitter that plays a significant role in mood regulation and cognitive functions. Following a head injury, dopamine dysregulation can occur, leading to various psychological challenges. Individuals may experience heightened feelings of fatigue, irritability, or apathy as their brain struggles to maintain normal dopamine levels.
This imbalance not only affects emotional well-being but also impacts cognitive performance. Difficulty concentrating and processing information are common complaints among those with disrupted dopamine pathways. Tasks requiring focus might become daunting or even frustrating.
Furthermore, the relationship between dopamine and reward systems means individuals may lose interest in activities they once enjoyed. This anhedonia can exacerbate feelings of sadness or hopelessness post-injury.
Restoring proper dopamine function is essential for recovery. Understanding these effects can help guide treatment strategies aimed at addressing both mood disturbances and cognitive deficits following head trauma.
Serotonin Imbalance and Its Relationship to Post-Concussion Depression
Serotonin plays a crucial role in regulating mood, emotions, and overall mental well-being. After a head injury, serotonin levels can become disrupted, contributing to various psychological symptoms. This disruption is particularly significant as it relates to post-concussion depression.
Research indicates that lower serotonin levels may heighten the risk of developing depressive symptoms following a concussion. Affected individuals might experience feelings of sadness or hopelessness that stem not only from their circumstances but also from biochemical changes in the brain.
This imbalance can lead to irritability, fatigue, and difficulty concentrating—further complicating recovery efforts. The interplay between serotonin and other neurotransmitters adds another layer of complexity to understanding these mood disturbances.
Addressing this imbalance becomes vital for effective recovery strategies. Therapeutic interventions aimed at boosting serotonin levels could provide relief for those grappling with post-concussion depression while improving overall emotional health during rehabilitation.
GABA Alterations: Implications for Anxiety and Sleep Disturbances
GABA, or gamma-aminobutyric acid, is a crucial neurotransmitter that helps regulate brain excitability. Following a head injury, GABA levels can become disrupted. This alteration often leads to increased anxiety and challenges with sleep regulation.
When GABA is diminished, the balance between excitation and inhibition in the brain shifts dangerously. Individuals may experience heightened feelings of stress and unease. The soothing effects of GABA are essential for promoting relaxation; without adequate levels, anxiety symptoms can escalate.
Sleep disturbances are another significant concern associated with altered GABA function. People struggling with low GABA levels may find it difficult to fall asleep or stay asleep throughout the night. Insomnia or restless nights not only affect daily performance but also contribute to emotional instability.
Addressing these disruptions is vital for recovery after a head injury. Therapeutic approaches that enhance GABA activity could play an important role in restoring calmness and improving sleep quality as part of holistic post-injury care strategies.
Diagnostic Challenges in Assessing Neurotransmitter Imbalances
Assessing neurotransmitter imbalances after head injury presents significant diagnostic challenges. One major hurdle is the complexity of neurotransmitter systems themselves. These chemical messengers do not operate in isolation; they interact with each other and with various brain regions, making it difficult to pinpoint specific imbalances.
Additionally, traditional diagnostic tools often fall short. Blood tests may reveal limited information since most neurotransmitters are primarily active within the central nervous system. As a result, clinicians must rely on indirect methods such as symptom assessments and patient histories, which can be subjective.
Another challenge lies in the variability among individuals. Factors like genetics, pre-existing conditions, and lifestyle can influence how someone responds to an injury and their subsequent neurotransmitter levels. This means that two patients with similar injuries might experience vastly different symptoms due to unique biochemical responses.
Research into neuroimaging techniques is ongoing but still evolving. Advanced imaging could provide insights into brain chemistry but isn’t yet widely available for routine clinical use.
Pharmacological Approaches to Neurotransmitter Modulation
Pharmacological approaches to address neurotransmitter imbalances after head injury involve various medications designed to restore equilibrium in brain chemistry. These treatments target specific neurotransmitters, aiming to alleviate symptoms and promote recovery. For instance, antiepileptic drugs may help manage glutamate excitotoxicity by reducing excessive neuronal firing.
Dopamine agonists can be beneficial for individuals facing mood and cognitive issues stemming from dopamine dysregulation. By enhancing dopamine activity, these medications improve motivation and focus. Similarly, selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed for addressing post-concussion depression linked to serotonin imbalance.
GABAergic agents also play a crucial role in managing anxiety and sleep disturbances following head injuries. By increasing GABA levels or activity, they promote relaxation and improve sleep quality. Importantly, the choice of pharmacological intervention should always be tailored to individual needs based on specific neurotransmitter disruptions.
Combining medication with other therapeutic strategies often enhances effectiveness. This multi-faceted approach aims not only to mitigate symptoms but also support overall brain health during recovery.
Nutritional Strategies to Support Neurotransmitter Balance
Nutritional strategies play a crucial role in supporting neurotransmitter balance following a head injury. A well-rounded diet rich in essential nutrients can help restore optimal brain function. Foods high in omega-3 fatty acids, such as salmon and walnuts, are known to promote dopamine production while reducing inflammation.
Incorporating complex carbohydrates like whole grains provides sustained energy and aids serotonin synthesis. Foods that contain vitamin B6, including bananas and chickpeas, contribute to the production of neurotransmitters, particularly serotonin and dopamine. These vitamins are vital for mood regulation.
Antioxidant-rich fruits and vegetables also support brain health by combating oxidative stress caused by head injuries. Blueberries, spinach, and kale can enhance cognitive function through their protective properties.
Hydration is often overlooked but remains essential for maintaining overall brain health. Drinking sufficient water helps facilitate nutrient transport throughout the body, ensuring that neurotransmitter levels remain balanced during recovery from injury.
Long-Term Consequences of Persistent Neurotransmitter Disruptions
Persistent neurotransmitter imbalances after head injury can lead to significant long-term consequences that affect various aspects of life. Individuals may experience ongoing cognitive impairments, which can hinder their ability to concentrate, remember information, and make decisions. This cognitive fog often creates challenges in both personal and professional settings.
Mood disorders are another common outcome of these imbalances. Many individuals face debilitating anxiety or depression that stems from disrupted serotonin and dopamine levels. Such emotional struggles can diminish quality of life, making it difficult for affected individuals to engage socially or maintain relationships.
Sleep disturbances frequently arise as well due to GABA alterations. Poor sleep not only exacerbates mental health issues but also impedes the brain’s natural recovery processes following an injury.
Furthermore, chronic fatigue is a recurring theme among those with persistent neurotransmitter disruptions. This constant state of tiredness affects motivation, energy levels, and overall productivity.
Long-term monitoring and intervention become crucial for managing these effects effectively. Understanding how neurotransmitters influence recovery can guide tailored treatment strategies aimed at restoring balance and enhancing the rehabilitation journey post-head injury. Addressing these imbalances early on may significantly improve outcomes in the long run for many individuals navigating this challenging path.