Headaches can often feel like an all-too-common nuisance, but for those recovering from a concussion, they can take on a more complex and debilitating form. Post-traumatic headaches (PTH) are a significant concern in individuals who have suffered head injuries. Understanding the various types of post-traumatic headache and their management is crucial for effective recovery.
This comprehensive guide will delve into what PTH entails, how it classifies into acute or chronic forms, and the specific symptoms associated with different types such as migraine-like headaches and tension-type headaches. By gaining insight into these pain patterns, patients can better navigate treatment options—from medication to non-pharmacological approaches—aimed at alleviating their discomfort.
Whether you’re experiencing these symptoms yourself or supporting someone who is, this resource aims to empower you with knowledge about post-traumatic headache types and management strategies that promote healing and improve quality of life.
Understanding Post-Traumatic Headache (PTH) in Concussion Patients
Post-traumatic headache (PTH) is a common condition that arises following a concussion. It can significantly impact the recovery process, making understanding its nature essential for patients and caregivers alike. PTH may occur immediately after injury or develop over time.
The mechanisms behind PTH are multifaceted, often involving changes in brain function and inflammation resulting from the head trauma. This type of headache can vary widely in intensity and duration, creating challenges for both diagnosis and treatment.
Many individuals experience headaches that resemble migraines or tension-type headaches, but some might also report cervicogenic pain linked to neck injuries sustained during the incident. The variability in symptoms underscores the importance of personalized assessment by healthcare professionals.
Recognizing these factors allows for better management strategies tailored to individual needs, improving overall outcomes as patients navigate their post-concussion journey. Understanding how PTH affects daily life is crucial for fostering effective communication between patients and their medical teams.
Classifying Post-Traumatic Headache Types: Acute vs. Chronic
Post-traumatic headaches can vary significantly in duration and intensity. They are typically classified into two main categories: acute and chronic. Acute post-traumatic headaches occur within the first few days to weeks following a concussion or head injury. These headaches often resolve on their own as the brain heals, but they can still be quite debilitating during this period.
Chronic post-traumatic headaches, on the other hand, persist for three months or longer after a concussion. This type is more complex and may require comprehensive management strategies to alleviate symptoms effectively. Individuals suffering from chronic headaches may experience recurrent pain that affects daily activities and quality of life.
The distinction between these two types is crucial for establishing appropriate treatment plans. Understanding whether a headache is acute or chronic helps healthcare providers identify underlying mechanisms and tailor interventions accordingly. Timely diagnosis can lead to better outcomes for those affected by post-traumatic headache types.
Migraine-Like Post-Traumatic Headaches: Symptoms and Treatment
Migraine-like post-traumatic headaches can be particularly debilitating for individuals recovering from a concussion. These headaches often present with symptoms similar to traditional migraines, including throbbing pain typically on one side of the head, sensitivity to light and sound, and nausea. Patients may describe these attacks as severe enough to interfere with daily activities.
The onset of migraine-like headaches can occur within days or weeks following the traumatic event. Triggers may include physical activity, stress, hormonal changes, or even certain foods—all familiar culprits in typical migraines. Recognizing these triggers is essential for effective management.
Treatment options vary based on severity and frequency of attacks. Acute treatments like non-steroidal anti-inflammatory drugs (NSAIDs) are commonly recommended during an attack. Preventive medications such as beta-blockers or anticonvulsants might also help reduce their occurrence.
Lifestyle adjustments play a crucial role in managing these headaches. Maintaining regular sleep patterns, staying hydrated, and practicing relaxation techniques can significantly improve quality of life for those affected by migraine-like post-traumatic headaches.
Tension-Type Headaches Following Concussion
Tension-type headaches (TTH) are a common consequence of concussions. They can develop shortly after the injury or may arise weeks later as part of post-concussion syndrome. TTH is often characterized by a pressing or tightening sensation around the head, resembling a band-like pressure.
The pain tends to be mild to moderate and is usually bilateral, affecting both sides of the head. Unlike migraines, these headaches do not typically include nausea or vomiting but can still significantly impact daily life. Patients may experience sensitivity to light and sound, though it’s less severe than that associated with migraine attacks.
Stress, anxiety, and muscle tension in the neck and shoulders often exacerbate TTH following a concussion. These factors create additional strain on already sensitive areas post-injury. Identifying triggers is crucial for effective management.
Treatment options include over-the-counter analgesics like ibuprofen or acetaminophen. Physical therapy focusing on relaxation techniques and posture correction can also help alleviate symptoms over time.
Cervicogenic Headaches: The Neck-Head Pain Connection
Cervicogenic headaches originate from issues in the cervical spine or neck region. They can often be mistaken for other headache types, especially after a concussion. The pain usually starts at the base of the skull and can radiate to various areas, including the forehead, temples, and even behind the eyes.
These headaches are frequently triggered by neck movements or certain postures. Activities such as prolonged sitting with poor posture or sudden jerking motions may exacerbate symptoms. As muscles tighten around injury sites, they can further amplify discomfort.
Identifying cervicogenic headaches involves assessing both the head and neck for dysfunctions. Healthcare providers may perform physical examinations to evaluate range of motion and tenderness in specific areas.
Treatment options typically focus on addressing underlying cervical issues through physical therapy, chiropractic care, or targeted exercises aimed at restoring mobility and reducing muscle tension. In some cases, injections may be recommended to alleviate persistent pain originating from nerve irritation in the neck.
Medication Overuse Headaches in Post-Concussion Syndrome
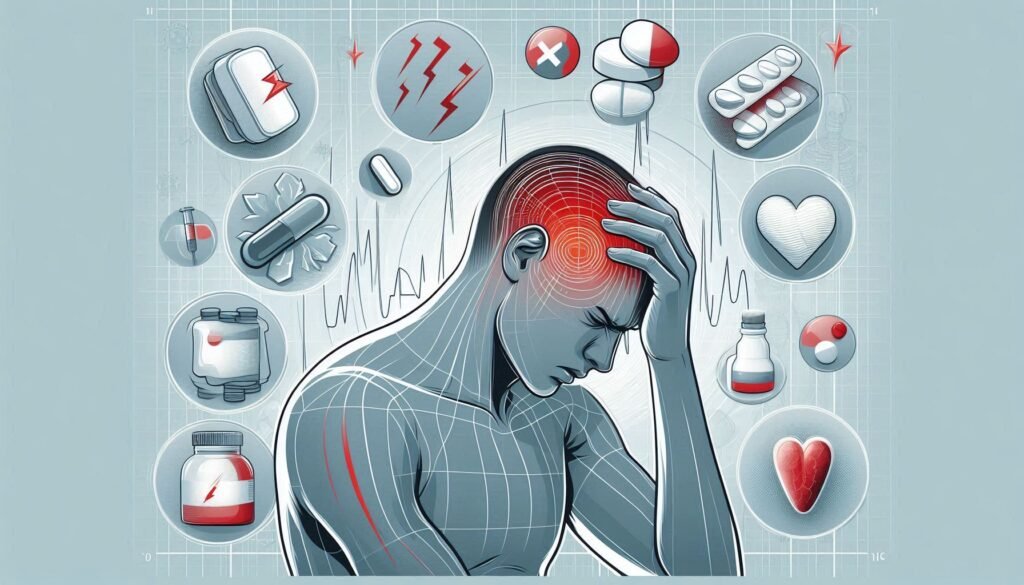
Medication overuse headaches (MOH) can be a significant complication for individuals suffering from post-concussion syndrome. These headaches often arise when patients excessively use pain relief medications, such as opioids or non-steroidal anti-inflammatory drugs (NSAIDs), in an attempt to manage their symptoms. The irony is that while these medications provide temporary relief, they can lead to increased headache frequency and intensity.
Patients may not realize they are developing MOH until the pain becomes more persistent. Symptoms typically include daily or near-daily headaches that can mimic other headache types but are often less responsive to usual treatments. This cycle of reliance on medication creates a frustrating paradox for those already struggling with concussion-related issues.
Preventing MOH requires careful monitoring of medication use and establishing clear guidelines for treatment duration. Educating patients about the risks associated with overusing pain relievers is crucial in managing this condition effectively.
When addressing MOH, healthcare providers must consider alternative therapies alongside proper medication management strategies.
Non-Pharmacological Approaches to PTH Management
Non-pharmacological approaches to managing post-traumatic headaches (PTH) can be highly effective. These methods often focus on lifestyle changes and therapeutic interventions, providing relief without the side effects associated with medications.
Cognitive-behavioral therapy (CBT) is one popular option. It helps patients identify triggers and develop coping strategies. This psychological approach can significantly reduce headache frequency and intensity by addressing underlying stressors.
Physical therapy also plays a crucial role in PTH management. Tailored exercises strengthen neck muscles, improve posture, and enhance mobility. Such improvements can alleviate tension in the cervical region that may contribute to headaches.
Mindfulness techniques, including meditation and yoga, are valuable as well. They promote relaxation and stress reduction while enhancing overall mental well-being. By incorporating these practices into daily routines, patients often experience fewer headaches over time.
Botulinum Toxin Injections for Chronic Post-Traumatic Headache
Botulinum toxin injections, commonly known as Botox, have emerged as a promising treatment for chronic post-traumatic headaches (PTH). This approach is particularly beneficial for patients who do not respond well to traditional headache medications. The injections work by blocking the release of certain neurotransmitters that contribute to pain signaling.
Patients receive multiple small injections in specific areas around the head and neck. These targeted sites often include muscles responsible for tension and pain. Clinical studies have shown significant reductions in headache frequency and intensity following this treatment.
The effects of botulinum toxin can last several months, making it an appealing option for those suffering from persistent symptoms. It may take time to observe its full benefits; however, many report improvements after just one or two sessions.
While side effects are generally mild, such as temporary bruising at the injection site, it’s essential to consult with a healthcare provider experienced in administering these treatments. Personalized assessment ensures optimal results tailored to each patient’s unique needs.
The Role of Neuroimaging in Diagnosing Post-Traumatic Headaches
Neuroimaging plays a crucial role in diagnosing post-traumatic headaches. Advanced imaging techniques, such as MRI and CT scans, help visualize the brain’s structure. These images can reveal abnormalities that may contribute to headache symptoms. For example, they can detect bleeding or swelling following trauma.
Not all headaches necessitate neuroimaging; however, specific red flags prompt healthcare providers to order these tests. Symptoms like severe pain, neurological deficits, or changes in consciousness warrant further investigation through imaging. Understanding the underlying causes of headaches is essential for effective management.
Moreover, neuroimaging aids in ruling out secondary causes of headache unrelated to trauma. Conditions such as tumors or vascular issues can mimic post-traumatic headache symptoms but require different treatment approaches. By eliminating these possibilities early on, patients receive focused care tailored to their needs.
Neuroimaging enhances diagnostic accuracy and guides clinicians in creating appropriate treatment plans for individuals experiencing post-traumatic headaches following concussion events.
Developing a Comprehensive Treatment Plan for PTH Patients
Developing a comprehensive treatment plan for post-traumatic headache (PTH) patients is crucial for effective management. Each patient presents unique symptoms and histories, necessitating a tailored approach. Collaboration among healthcare providers—including neurologists, physical therapists, and psychologists—can enhance treatment efficacy.
A thorough assessment should include detailed medical histories and specific symptom evaluations to identify the type of PTH present. This will inform whether acute or chronic strategies are more appropriate. Treatment options may involve pharmacological methods such as preventive medications or targeted therapies based on headache classification.
In addition to medication, integrating non-pharmacological approaches can provide significant relief. Techniques like cognitive-behavioral therapy (CBT), relaxation exercises, biofeedback training, and lifestyle modifications play vital roles in managing headaches effectively.
Regular follow-ups are essential to adjust treatments as needed and monitor progress over time. Encouraging open communication between patients and their healthcare team fosters trust and ensures that individual needs are met throughout recovery.
When properly addressed with an individualized strategy combining various modalities, many patients find substantial improvement in quality of life after experiencing post-traumatic headaches following concussion events.